Your Health Department is Prepared
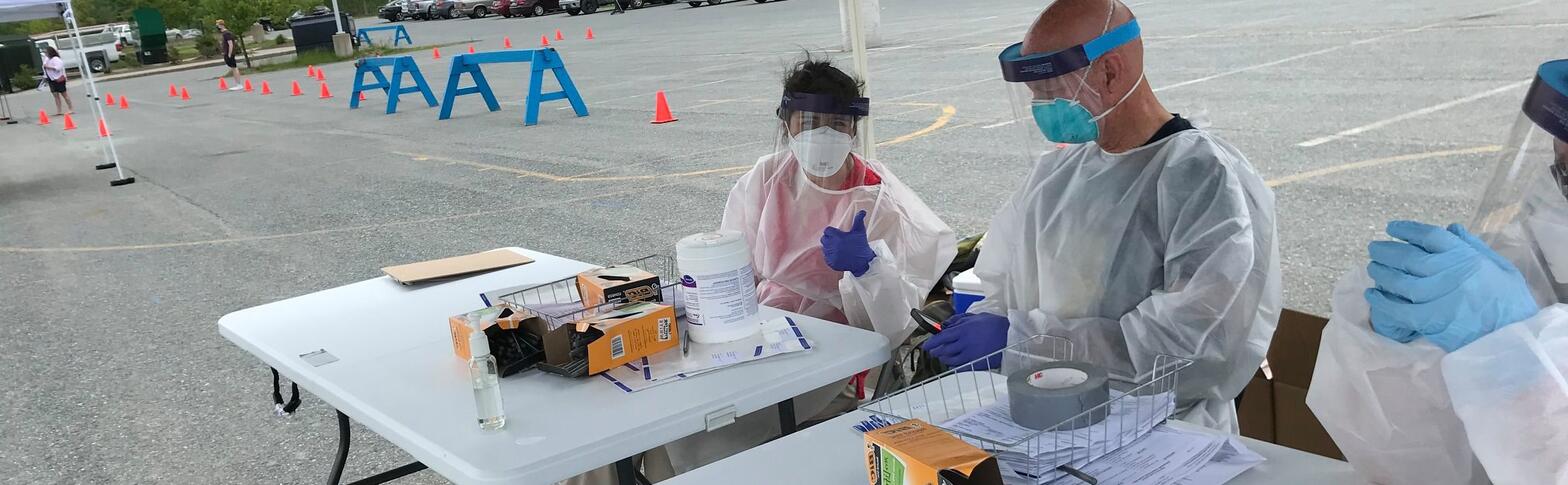
When facing an infectious disease outbreak or pandemic, natural or man-made disaster, environmental hazard, extreme weather or other health crisis, the Vermont Department of Health is prepared to respond quickly and effectively.
We use our Health Operations Center and Incident Command Structure to organize our response. We work with other government agencies, hospitals, health care providers, EMS, first responders and community partners to respond to – and recover from – events and emergencies that threaten the health and safety of people who live in Vermont.