Mpox—previously referred to as monkeypox or hMPXV— continues to circulate in the U.S. Take steps to prevent getting mpox, including getting vaccinated if you're at risk.
There are two kinds of mpox, clade I and clade II. Clade I usually causes more people with mpox to get severely sick or die compared to clade II. Mpox clade II continues to spread in many countries around the world, including the U.S. Mpox clade I is currently spreading mainly in certain countries in Africa.
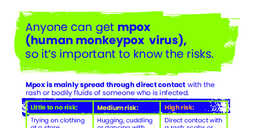
Mpox is a viral illness that is mainly spread through close, personal (skin-to-skin) contact with someone who is infected. The most common symptom is a rash, which may look like pimples, blisters, or sores, or other more common rashes such as chicken pox, syphilis, or shingles. The rash can be extremely painful and leave scars. Other symptoms may include fever, headache, muscle aches, backaches, swollen lymph nodes, chills, and exhaustion.
Talk to your health care provider if you have a rash or other symptoms of mpox—even if you have been vaccinated or had mpox before. If you do not have a health care provider, call 2-1-1 to be connected to care, or contact the nearest federally qualified health center or one of Vermont's Free & Referral Clinics.
Find translated videos and factsheets in: American Sign Language / العربية / Arabic မြန်မာစာ / Burmese دری / Dari Français / French Kirundi Maay Maay Mandarin Chinese नेपाली / Nepali پښتو / Pashto Soomaali / Somali Español / Spanish Swahili українська / Ukrainian Tiếng Việt / Vietnamese